Professor Improving Joint Replacements With $2 Million Grant
One of the most common sources of discomfort for U.S. senior citizens is osteoarthritis (OA). The “wear and tear” chronic joint condition frequently requires knee and hip replacements just to mediate the pain, stiffness and swelling. According to Kevin Shelburne, a research professor at the Ritchie School of Engineering & Computer Science, the treatment is largely effective: only 5–10 percent of patients are dissatisfied with the surgery.
“That doesn’t sound like a lot,” Shelburne says, “until you consider that there are 860,000 of these [surgeries] every year.”
And considering that OA already affects 30 million Americans — a figure expected to rise with an increasingly obese and elderly population — Shelburne knows there is room to improve the metal or plastic pieces inserted to reduce pain.
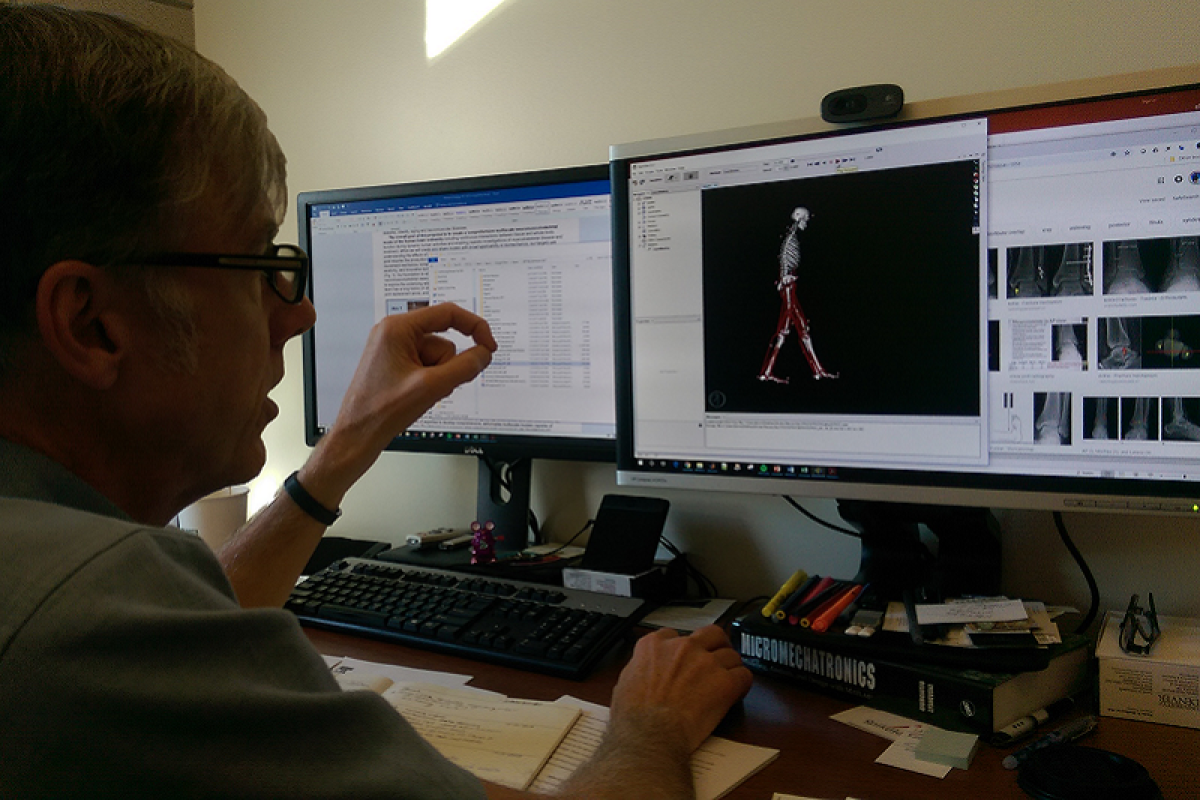
With a nearly $2 million grant from the National Institutes of Health (NIH) and state-of-the-art facilities at the University of Denver, Shelburne and a team of researchers are working toward a better solution. The goal is to create a new computer model of humans and their movement, providing joint replacement designers the information they need to build a better product.
Current computer software shows a simple representation of the muscles, bones and other tissues of the human body. These models simulate a single generic person and predict the impact various forces and movements will have on the joints.
“If you had computer models that were sophisticated enough and could represent a range in population, it could go a long way toward helping develop new treatments,” Shelburne says. “What we want to do is add more realism to the models. We want something that’s actually representing the true geometry, the deformability of the muscle. And not just the muscle but the ligaments as well, the tendons and some of the fat.”
Any solution must be multiscale, Shelburne says, meaning it must examine the way various parts of the body interact. “You can have a very small injury in your knee or hip or shoulder, and it’s going to affect your whole body motion,” he says. Pain in one area can cause a person to overcompensate and change the way they move, he adds. That adjustment must be taken into account.










