New Healthcare Management Offerings ‘Peel Back the Onion’ on Health Equity and Justice

Disparities in patient care have been an issue in the health care industry for decades, but the COVID-19 pandemic thrust the need for change front and center—and University College, the University of Denver’s hub for continuing and professional education, is stepping up to respond to the demand.
Last November, the college added the Advancing Diversity, Equity and Inclusion in Organizations (ADEIO) concentration to its master’s degree program in health care management. In addition to the five core courses and three electives that make up the program, the ADEIO concentration includes four courses that build cultural competency: Culture, Identity and Power; Diversity and Organizational Structure; The Inclusive Organization; and Leading Change for Transformation.
“It became evident, from industry partners, professional organizations and our advisory board members, that [DEI] is a skill and a competency and an understanding that health care professionals and leaders all over the state and country are looking for,” says Rachel Rogers, academic director of the program.
The four ADEIO courses are “industry-agnostic” and part of the curriculum in other degree programs at the college, including Strategic Human Resources and Global Community Engagement. Rogers was determined, however, to add a course focused specifically on the role of DEI in health care—and so this fall, students will also have the option of taking a new course, Health Equity and Social Justice, as an elective.
“It was important to me to call out how the health care system itself contributes to disparities,” says Rogers. “I wanted to look at it from the provider to patient perspective, which is what this class really does. How can we think more clearly about the structural pieces that have contributed … and how do we fix the disparities that we know exist?”
Rogers recruited two nurse leaders from a Denver hospital, Debra Gardner and Tonie Moore, to develop and teach the 10-week course. The two colleagues had never designed a course before, but they were eager to dig into the research examining what they have experienced firsthand working in a safety-net hospital that serves all patients, regardless of insurance status or ability to pay.
“As a nurse, you always recognize that we have these glaring problems with inequity in the systems. You can see it when you look around at who you work with and how you care for your patients,” Gardner says. “The pandemic, though, really peeled the layers on that onion [in terms of] learning and seeing things very differently.”
During COVID, she says, the disparities “were right in front of our faces. It wasn’t a statistic, it was life, every single day. We’re going to meetings and people are saying, ‘My ICUs are full of people of color dying.’” In addition, she says, the pandemic highlighted disparities among the health care professionals themselves. “It was really painful … how you have diverse teams that struggle to work together and people feeling unwelcome and how patient care really suffers from that.”
The challenge, Gardner says, is to make changes that are “real and not just performative.” When she and Moore began researching for the course and learned about the social justice model, they knew they had found the right framework.
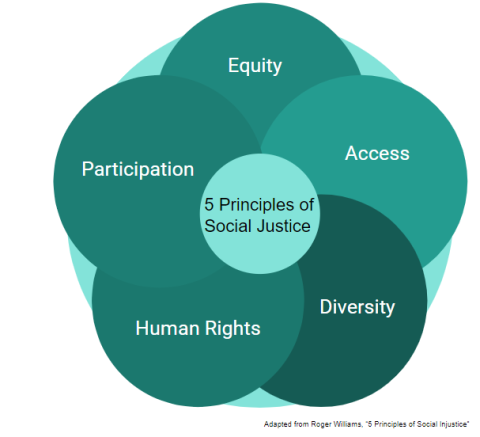
The model is built on five principals—access to resources, equity, participation, diversity and human rights—and lays the foundation for a curriculum that looks at the structure of biases in the health care system, as well as at the experiences of the individual provider and, most importantly, the patient.
“In the health care environment, we become desensitized to a lot of things,” Moore says. “It’s important to understand the patient’s background, their history, the environment in which they’re currently living—to understand who I’m coming into contact with as a provider.” She adds that this includes not just patients of color but also the disabled, the elderly and non-native English speakers.
Gardner and Moore say they selected resources and activities that would raise student awareness of the issues while engaging them on a personal level—including recording a video journal of their thoughts and reactions throughout the course, listening to podcasts and watching documentaries such as “Crip Camp” and “Romeo Is Bleeding.”
The two also want to be sure, Gardner says, that students understand “they don’t have to champion this by themselves.” They will learn how to be an advocate and how to work effectively with teams and partners. Activities will include interviewing a health care leader, researching a local community organization and designing an intervention for a specific population.
The team hopes that, by the end of the program, students will become more self-aware and better equipped to make meaningful changes. Says Rogers, “We want students to think about their own socialization, what they have been raised and trained to think, and how they might need to think differently in order to deliver care in a way that acknowledges the value in each person—and how that care gets delivered and how to bring it to scale across systems and populations.”